Here’s How New Paramedics Should Be Interpreting ECGs
Sometimes ECG interpretation is hard.
In the field strips don’t look like they should. People are moving, leads aren’t sticking right. It can be a mess.

But whenever we don’t know where to go, we need to fall back on our basics.
I’m Shay. I’ve been working in pre-hospital EMS for 13 years.
Let me show you how I still read all my ECG strips as a paramedic.
It’s only a few easy steps and will quickly point you in the right direction for interpreting a strip.
How to Read an ECG Strip

Here are the five things I do every time to read an ECG strip.
- Measure the Rate
- Regular or Irregular
- Find your P Waves
- Measure QRS
- Check ST Segment
- Identify the Rhythm
Each of these steps is pretty simple once you get some practice. It’s just a matter of putting it all together.
If you can tell me the rate, if it’s regular, and how wide the QRS complex is, I bet you can correctly identify the rhythm.
Even if you can’t, you’re a lot closer to a successful treatment than you were before.
And that’s always the goal. We want to give our patients the best chance for a good outcome.
So let’s go over each step, one at a time. You should be able to perform each step quickly and efficiently.
From there you can really narrow down what treatments are available to you.
Start with Heart Rate
The heart rate can tell you a lot right off the bat.
Once I determine whether the rate is too fast or too slow, I can focus the rest of my investigation.

How do we tell the rate?
There’s a few ways. Of course we could just find the pulse and see how many beats we get in six seconds.
Multiply that by ten and you have your beats per minute.
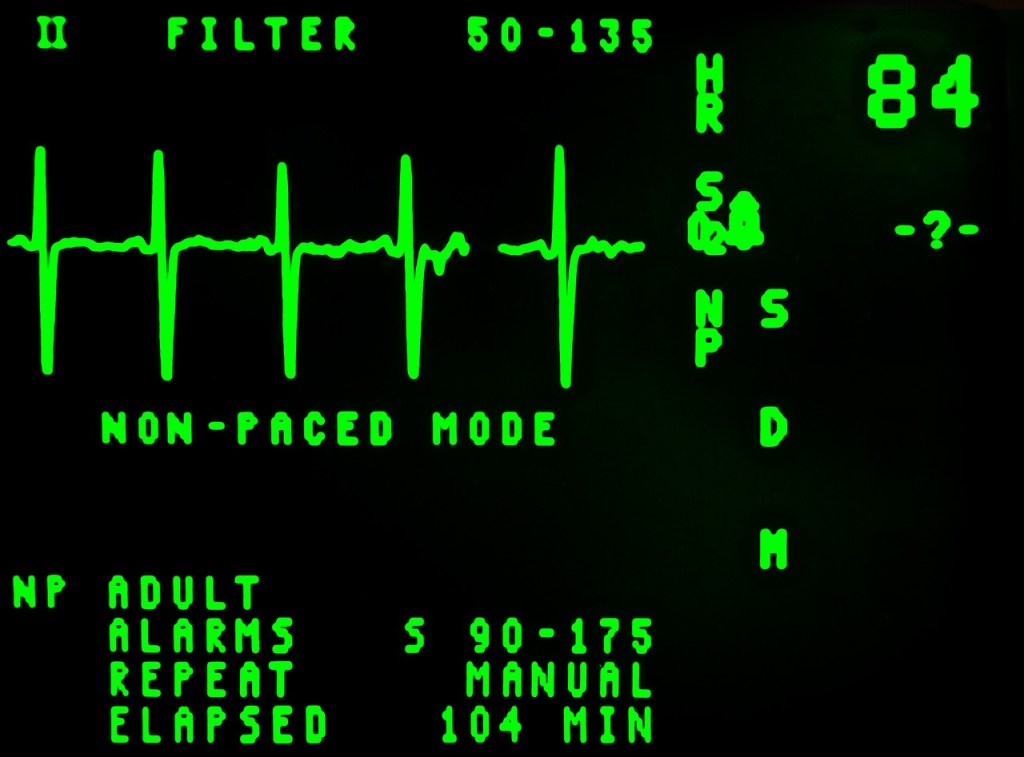
We could also find it on our monitor.
Most cardiac monitors will give you a read out of the heart rate in an easy to read number.
Remember, if the number is jumping all over the place, it’s probably an irregular rhythm.
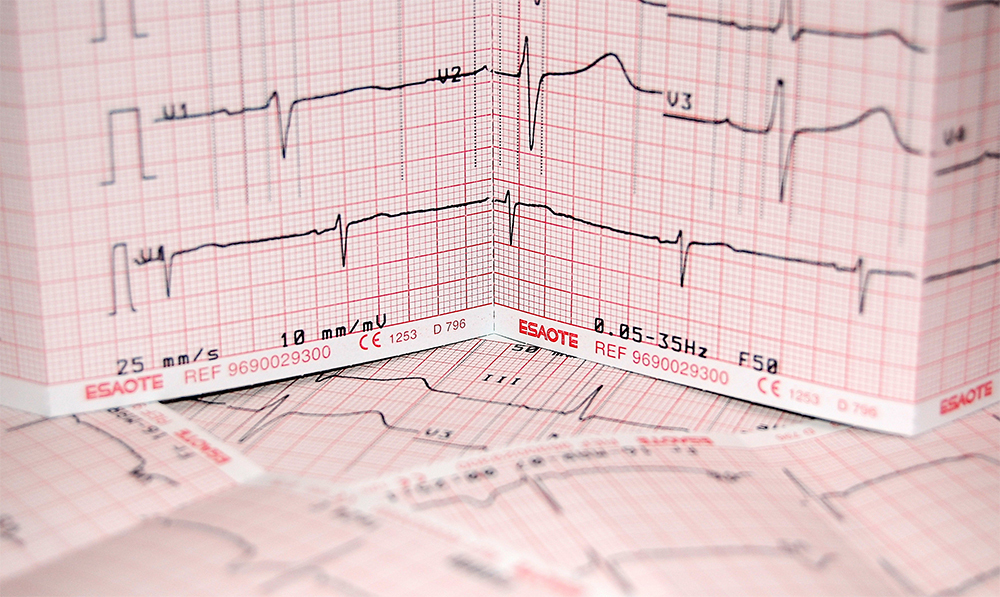
What if we only have an EKG strip?
The heart rate is pretty easy to find here too. All we need to do is count the boxes between QRS complexes.
One large box between strips is 300 BPM. Pretty fast.
Two large boxes is 150 BPM.
Three large boxes between complexes is 100 BPM.
Four is 75 BPM. Five is 60 BPM.
Notice a pattern? Its 300 divided by the number of large boxes between QRS complexes.
To get our rate of 60 BPM you take 300 and divide it by five large boxes.
Its a really down and dirty way to find a heart rate on an EKG. It’s only reliable if the rate is regular.
Which leads us to step 2.

Regular or Irregular Rate
This is really easy. Does the QRS fire off in a consistent rate? It’s regular.
If you can’t quickly determine when the next QRS will show up the rate is irregular. It really is that easy.
Now your rate can be slow or fast and regular or irregular.
But those two things have already narrowed down what is happening to my patient.
It also tells you what treatment algorithms to start going down.

Bonus point, if your rate is irregular you do need to march out a ten second strip on your EKG and multiply by six.
It’s a much more accurate representation of rate that using the box method.
Find Your P Waves
Next we need to see if your rhythm is sinus or not.
Sinus just means it originates from the sinoatrial (SA) node in the right atrium.
Every P Wave should be followed by a QRS complex.
If it isn’t, we have a few options. The most common causes are heart blocks and Atrial Fibrillation.

If you have a ton of P Waves but only a few jumbled QRS complexes, congrats, your patient is in A-Fib. If the rate is too fast you’ve got A-fib with rapid ventricular response.
Wow, we’re already diagnosing the rhythm and we haven’t even made it to step four.
Heart blocks are another common reason for QRS complexes to be dissociated from your P Waves. We won’t dive too much into them right now, though.
Otherwise we would be here all day.
To put it simply, find your P Waves and see if everyone has a QRS after it.
Measure the QRS
The QRS width on an ECG can tell you a lot of things about your patient’s heart.
I find it easiest to think about QRS width in the context of tachycardia or bradycardia.
That’s because the treatment for these rhythms is very different depending on whether they are narrow or wide.
A wide QRS- greater than 0.1 s- means the electricity is taking a weird path through the heart.
Obviously, that’s not good.

A normal QRS should be 0.04 – 0.1 s. This looks like 2 – 5 little boxes on your EKG strip. Or half a big box.
A wide QRS complex in a bradycardic rhythm tells you the heart is beating off a ventricular pacemaker cell.
Thats not good. The ventricle naturally beats too slowly.
And the treatment for that rhythm is different than a sinus bradycardic rhythm with a normal QRS.
Again, no treatments today. You’re just worrying about rhythm identification.

ST Elevation or Depression
Here’s the big one. Is our patient having a heart attack?
After everything else we look to that little segment between the QRS complex and T Wave. Thats called the ST Segment.
Original name, I know.
You want to see if it is elevated 2 or more boxes above the isoelectric line. Thats the flat line you see between beats.
Having two consecutive leads with 2 or more boxes means you have a STEMI. Thats ST segment Elevation Myocardial Infarction.

Or you could just call it a heart attack.
You might also see ST depression.
This doesn’t necessarily mean they are having a heart attack. It does mean something bad is happening with your pateint.
ST depression occurs when your patient’s heart isn’t getting enough oxygen. Cardiac ischemia is bad news.
Final Point. Not every heart attack has ST elevation.
You can have an N-STEMI (Non-ST Elevation Myocardial Infarction).
That’s why you always transport chest pain patients.
Blood work is the definitive answer to whether or not your patient is having a cardiac event.

Naming Your Rhythm
So you went through all the steps. Found the rate and figured out if it was irregular or not. Checked your P-Waves. Measured your QRS. Looked at the ST Segment.
Now you need to put it all together and name that rhythm
Name That Rhythm. That would be a fun game show.
Anyway, let’s take an example. Say you found your patient’s rate was 160 BPM. It was irregular and you had to count out all the QRS complexes in a 6 second strip to get that.

Then we looked at the P Waves. There were a lot of them but they didn’t always have a QRS. You should already know how to name this rhythm.
But next step, look at the QRS complex. Oh look, it’s less than 0.1 seconds long so it’s a narrow complex tachycardia.
Looking at the ST segment last, we see some depression but no elevation.
Cool. Let’s name it.
We have A-Fib with a rapid ventricular response with noted ST-depression.
BAM. Good for you. Now you can start your treatment algorithm.

Rapid EKGs
EKGs aren’t all that hard to read for paramedics. Yes you can go super in detail with them. But a lot of the time it’s gee wiz stuff that doesn’t change your treatment.
Here are those six steps again all in one place.
- Measure the Rate
- Regular or Irregular
- Find your P Waves
- Measure QRS
- Check ST Segment
- Identify the Rhythm
If you want to be a good paramedic, really focus on the things you can change. And know what you just need to get to the ER. Fast.

I hope these steps helped. They have helped me in the field and it’s how I still look at all my ECG strips. If you liked them send me an Email at themedicsmentor@gmail.com
And you can find all our recommended study materials here on our site.
Have a safe shift!

Leave a comment