Mastering the Posterior 12-Lead ECG: A Paramedic’s Guide
Tired of missing those sneaky Posterior MIs?
As a paramedic, you’re on the front lines of emergency medicine. You’re tasked with making quick, accurate diagnoses to provide timely and effective care. One tool that can be incredibly helpful in your arsenal is the posterior 12-lead ECG.
So, when should you consider using a posterior 12-lead ECG?
The primary indication for a posterior 12-lead ECG is when you suspect a Posterior Wall Myocardial Infarction (PMI). This type of heart attack often presents with atypical symptoms, making it difficult to diagnose with a standard 12-lead ECG alone.
Why is a Posterior MI So Tricky?
The posterior wall of the heart is located on the back side, making it challenging to directly assess with standard ECG leads. This is because the electrical activity from the posterior wall is often obscured by the electrical activity from the anterior wall.
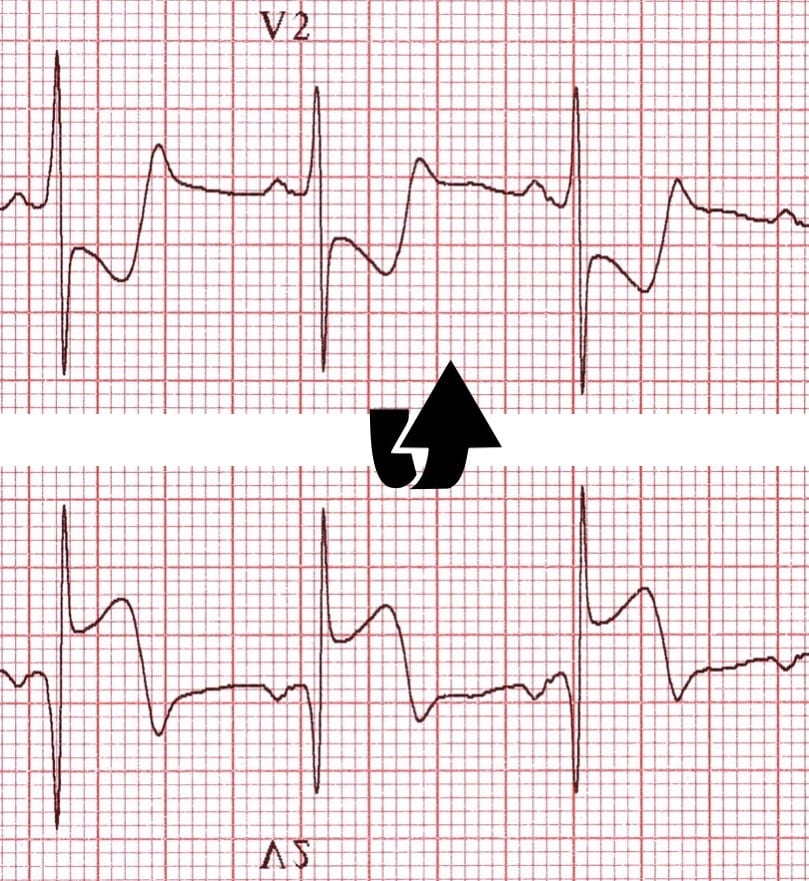
The Classic Signs: ST-Segment Depression in V1 and V2
One of the classic signs of a Posterior MI is ST-segment depression in leads V1 and V2. This occurs because the electrical activity from the injured posterior wall can influence the electrical activity recorded in these anterior leads.
Other Clues: Tall R Waves in V1 and V2
Another clue that may suggest a Posterior MI is the presence of tall R waves in leads V1 and V2. These tall R waves can be a result of the electrical activity from the injured posterior wall being conducted through the septum and recorded in these anterior leads.
When to Suspect a Posterior MI
Here are some clinical scenarios where you should consider a posterior 12-lead ECG:
- Atypical Chest Pain: If a patient presents with chest pain that is not typical of a classic anterior wall MI (e.g., pain radiating to the back or jaw), a posterior MI should be considered.
- Shortness of Breath: Shortness of breath can be a presenting symptom of a Posterior MI, especially in older adults or those with underlying cardiac conditions.
- Diaphoresis, Nausea, and Vomiting: These symptoms can accompany a heart attack, even if the chest pain is less severe or atypical.
Performing a Posterior 12-Lead ECG
To perform a posterior 12-lead ECG, you’ll need to place three additional electrodes: V7, V8, and V9. Here’s a step-by-step guide:
- Prepare the Patient: Ensure the patient is comfortable and positioned appropriately.
- Place Standard 12-Lead Electrodes: Attach the standard 10 electrodes as you would for a routine 12-lead ECG.
- Position Posterior Electrodes:
- V7: Place this electrode at the level of the fifth intercostal space, posterior axillary line.
- V8: Place this electrode at the same level as V7, posterior midaxillary line.
- V9: Place this electrode at the same level as V7 and V8, posterior scapular line.
Interpreting a Posterior 12-Lead ECG
Once you’ve recorded the posterior 12-lead ECG, you’ll need to interpret the results. Look for ST-segment elevation in leads V7, V8, and V9. This elevation indicates injury to the posterior wall of the heart.
Conclusion
By mastering the art of the posterior 12-lead ECG, you can significantly improve your ability to diagnose and treat patients with Posterior MIs. Remember, early recognition and intervention are crucial in optimizing patient outcomes.
Want more tips and tricks for new paramedics? You can find our full resource guide HERE
Leave a reply to 160,000 Posterior Heart Attacks Happen Every Year. Are You Missing These Subtle Posterior MI Criteria? – The Medic Mentor Cancel reply